FAQs about HALAVEN® for advanced liposarcoma
-
Who is the appropriate patient for HALAVEN?


HALAVEN (eribulin mesylate) Injection is indicated for the treatment of patients with unresectable or metastatic liposarcoma who have received a prior anthracycline-containing regimen.
-
What is some of the Important Safety Information I need to know about HALAVEN?


Warnings and Precautions
Neutropenia: Severe neutropenia (ANC <500/mm3) lasting >1 week occurred in 12% of patients with liposarcoma or leiomyosarcoma. Febrile neutropenia occurred in 0.9% of patients and fatal neutropenic sepsis occurred in 0.9% of patients. Monitor complete blood cell counts prior to each dose, and increase the frequency of monitoring in patients who develop Grade 3 or 4 cytopenias. Delay administration and reduce subsequent doses in patients who experience febrile neutropenia or Grade 4 neutropenia lasting >7 days.
Peripheral Neuropathy: Grade 3 peripheral neuropathy occurred in 3.1% of patients with liposarcoma and leiomyosarcoma receiving HALAVEN and neuropathy lasting more than 60 days occurred in 58% (38/65) of patients who had neuropathy at the last treatment visit. Patients should be monitored for signs of peripheral motor and sensory neuropathy. Withhold HALAVEN in patients who experience Grade 3 or 4 peripheral neuropathy until resolution to Grade 2 or less.
Embryo-Fetal Toxicity: HALAVEN can cause fetal harm when administered to a pregnant woman. Advise females of reproductive potential to use effective contraception during treatment with HALAVEN and for at least 2 weeks following the final dose. Advise males with female partners of reproductive potential to use effective contraception during treatment with HALAVEN and for 3.5 months following the final dose.
QT Prolongation: Monitor for prolonged QT intervals in patients with congestive heart failure, bradyarrhythmias, drugs known to prolong the QT interval, and electrolyte abnormalities. Correct hypokalemia or hypomagnesemia prior to initiating HALAVEN and monitor these electrolytes periodically during therapy. Avoid in patients with congenital long QT syndrome.
Adverse Reactions
In patients with liposarcoma and leiomyosarcoma receiving HALAVEN, the most common adverse reactions (≥25%) reported in patients receiving HALAVEN were fatigue (62%), nausea (41%), alopecia (35%), constipation (32%), peripheral neuropathy (29%), abdominal pain (29%), and pyrexia (28%). The most common (≥5%) Grade 3-4 laboratory abnormalities reported in patients receiving HALAVEN were neutropenia (32%), hypokalemia (5.4%), and hypocalcemia (5%). Neutropenia (4.9%) and pyrexia (4.5%) were the most common serious adverse reactions. The most common adverse reactions resulting in discontinuation were fatigue and thrombocytopenia (0.9% each).
Use in Specific Populations
Lactation: Because of the potential for serious adverse reactions in breastfed infants from eribulin mesylate, advise women not to breastfeed during treatment with HALAVEN and for 2 weeks after the final dose.
Hepatic and Renal Impairment: A reduction in starting dose is recommended for patients with mild or moderate hepatic impairment and/or moderate or severe renal impairment.
-
How was HALAVEN studied in patients with advanced liposarcoma?


The efficacy and safety of HALAVEN were evaluated in an open-label, randomized (1:1), multicenter, active-controlled trial. Eligible patients were required to have unresectable, locally advanced, or metastatic liposarcoma or leiomyosarcoma, at least 2 prior systemic chemotherapies (one of which must have included an anthracycline), and disease progression within 6 months of the most recent chemotherapy regimen. Patients were randomized to HALAVEN 1.4 mg/m2 administered intravenously on Days 1 and 8 of a 21-day cycle or to dacarbazine at a dose of 850 mg/m2, 1,000 mg/m2, or 1,200 mg/m2 administered intravenously every 21 days (dacarbazine dose was selected by the investigator prior to randomization). Treatment continued until disease progression or unacceptable toxicity. Randomization was stratified by histology (liposarcoma or leiomyosarcoma), number of prior therapies (2 vs >2), and geographic region. The most common (>40%) prior systemic chemotherapies were doxorubicin (90%), ifosfamide (62%), gemcitabine (59%), trabectedin (50%), and docetaxel (48%).1
-
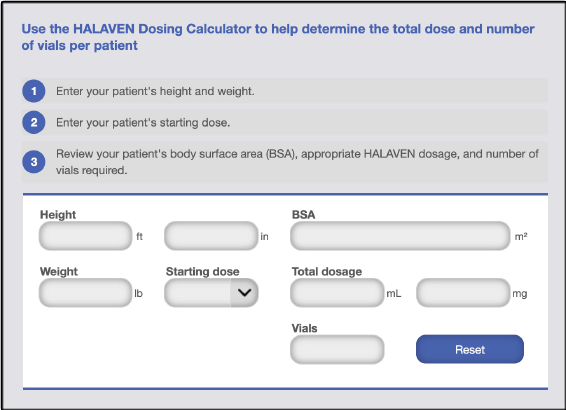
What is the recommended starting dose for HALAVEN?


HALAVEN is administered at 1.4 mg/m2 IV over 2 to 5 minutes on Days 1 and 8 of a 21-day cycle. The recommended dose of HALAVEN in patients with advanced liposarcoma who have mild hepatic impairment (Child-Pugh A) is 1.1 mg/m2. For patients with advanced liposarcoma who have moderate hepatic impairment (Child-Pugh B), the recommended dose of HALAVEN is 0.7 mg/m2. Finally, for patients with advanced liposarcoma who have moderate or severe renal impairment, defined as having a creatinine clearance of 15 mL/min to 49 mL/min, the recommended dose of HALAVEN is 1.1 mg/m2 over 2 to 5 minutes on Days 1 and 8 of a 21-day cycle.1
-
What do I need to know about HALAVEN dose modifications?


Patients with advanced liposarcoma should be assessed for peripheral neuropathy, and complete blood cell counts should be obtained prior to each dose.1
HALAVEN should not be administered on Days 1 or 8 for an absolute neutrophil count (ANC) of less than 1,000/mm3, platelets less than 75,000/mm3, or Grade 3 or 4 nonhematologic toxicities. The Day 8 dose may be delayed for a maximum of 1 week. However, if toxicities do not resolve or improve to Grade 2 or less in severity by Day 15, omit the dose. If toxicities resolve or improve to Grade 2 or less in severity by Day 15, administer HALAVEN at a reduced dose and initiate the next cycle no sooner than 2 weeks later.1
If a dose has been delayed for toxicities and toxicities have recovered to ≤Grade 2, HALAVEN may be resumed at a permanently reduced dose of 1.1 mg/m2 if any of the following occur: ANC is less than 500/mm3 for more than 7 days, ANC is less than 1,000/mm3 with fever or infection, platelets are less than 25,000/mm3, platelets are less than 50,000/mm3 requiring transfusion, nonhematologic Grade 3 or 4 toxicities, or omission or delay of Day 8 HALAVEN dose in previous cycle for toxicity.1
For any event requiring permanent dose reduction while receiving the 1.1 mg/m2 dose, HALAVEN may be resumed at a permanently reduced dose of 0.7 mg/m2 once toxicities have recovered to ≤Grade 2. Discontinue HALAVEN for any event requiring permanent dose reduction while receiving the 0.7 mg/m2 dose.1
-
How is HALAVEN believed to work?


Based on preclinical studies, with its distinct binding profile, HALAVEN causes irreversible mitotic blockage resulting in apoptosis, leading to the destruction of many tumor cells. Additionally, based on preclinical studies in human breast cancer models, HALAVEN causes vascular remodeling, reducing hypoxic conditions within the tumor and promoting the epithelial phenotype. This ultimately inhibits the migration and invasive capacity of residual breast cancer cells.1-8
-
Where can I find information on the HALAVEN $0 Co-Pay Program or reimbursement information for HALAVEN?


The HALAVEN $0 Co-Pay Program assists eligible commercially insured patients with the out-of-pocket costs of HALAVEN (co-payments and co-insurances). The $0 Co-Pay Program is part of the Eisai Assistance Program (EAP), which offers information about reimbursement and patient assistance programs. To learn more about the $0 Co-Pay Program and the EAP for HALAVEN, visit www.eisaireimbursement.com/hcp/halaven/patient-support or call 1.866.61.EISAI (1.866.613.4724) to speak with an EAP hotline agent (Monday to Friday, 8 AM to 8 PM ET).
Interactive resources
For questions about HALAVEN, e-mail Eisai Medical Information at Esi_oncmedinfo@eisai.com or call 1.888.274.2378
Indications
Metastatic Breast Cancer
HALAVEN (eribulin mesylate) Injection is indicated for the treatment of patients with metastatic breast cancer (mBC) who have previously received at least 2 chemotherapeutic regimens for the treatment of metastatic disease. Prior therapy should have included an anthracycline and a taxane in either the adjuvant or metastatic setting.
Liposarcoma
HALAVEN is indicated for the treatment of patients with unresectable or metastatic liposarcoma who have received a prior anthracycline-containing regimen.
Important Safety Information
Warnings and Precautions
Neutropenia: Severe neutropenia (ANC <500/mm3) lasting >1 week occurred in 12% of patients with mBC and liposarcoma or leiomyosarcoma. Febrile neutropenia occurred in 5% of patients with mBC and 2 patients (0.4%) died from complications. Febrile neutropenia occurred in 0.9% of patients with liposarcoma or leiomyosarcoma, and fatal neutropenic sepsis occurred in 0.9% of patients. Patients with mBC with elevated liver enzymes >3 × ULN and bilirubin >1.5 × ULN experienced a higher incidence of Grade 4 neutropenia and febrile neutropenia than patients with normal levels. Monitor complete blood cell counts prior to each dose, and increase the frequency of monitoring in patients who develop Grade 3 or 4 cytopenias. Delay administration and reduce subsequent doses in patients who experience febrile neutropenia or Grade 4 neutropenia lasting >7 days.
Peripheral Neuropathy: Grade 3 peripheral neuropathy occurred in 8% of patients with mBC (Grade 4=0.4%) and 22% developed a new or worsening neuropathy that had not recovered within a median follow-up duration of 269 days (range 25-662 days). Neuropathy lasting >1 year occurred in 5% of patients with mBC. Grade 3 peripheral neuropathy occurred in 3.1% of patients with liposarcoma and leiomyosarcoma receiving HALAVEN and neuropathy lasting more than 60 days occurred in 58% (38/65) of patients who had neuropathy at the last treatment visit. Patients should be monitored for signs of peripheral motor and sensory neuropathy. Withhold HALAVEN in patients who experience Grade 3 or 4 peripheral neuropathy until resolution to Grade 2 or less.
Embryo-Fetal Toxicity: HALAVEN can cause fetal harm when administered to a pregnant woman. Advise females of reproductive potential to use effective contraception during treatment with HALAVEN and for at least 2 weeks following the final dose. Advise males with female partners of reproductive potential to use effective contraception during treatment with HALAVEN and for 3.5 months following the final dose.
QT Prolongation: Monitor for prolonged QT intervals in patients with congestive heart failure, bradyarrhythmias, drugs known to prolong the QT interval, and electrolyte abnormalities. Correct hypokalemia or hypomagnesemia prior to initiating HALAVEN and monitor these electrolytes periodically during therapy. Avoid in patients with congenital long QT syndrome.
Adverse Reactions
In patients with mBC receiving HALAVEN, the most common adverse reactions (≥25%) were neutropenia (82%), anemia (58%), asthenia/fatigue (54%), alopecia (45%), peripheral neuropathy (35%), nausea (35%), and constipation (25%). Febrile neutropenia (4%) and neutropenia (2%) were the most common serious adverse reactions. The most common adverse reaction resulting in discontinuation was peripheral neuropathy (5%).
In patients with liposarcoma and leiomyosarcoma receiving HALAVEN, the most common adverse reactions (≥25%) reported in patients receiving HALAVEN were fatigue (62%), nausea (41%), alopecia (35%), constipation (32%), peripheral neuropathy (29%), abdominal pain (29%), and pyrexia (28%). The most common (≥5%) Grade 3-4 laboratory abnormalities reported in patients receiving HALAVEN were neutropenia (32%), hypokalemia (5.4%), and hypocalcemia (5%). Neutropenia (4.9%) and pyrexia (4.5%) were the most common serious adverse reactions. The most common adverse reactions resulting in discontinuation were fatigue and thrombocytopenia (0.9% each).
Use in Specific Populations
Lactation: Because of the potential for serious adverse reactions in breastfed infants from eribulin mesylate, advise women not to breastfeed during treatment with HALAVEN and for 2 weeks after the final dose.
Hepatic and Renal Impairment: A reduction in starting dose is recommended for patients with mild or moderate hepatic impairment and/or moderate or severe renal impairment.
Indications
Metastatic Breast Cancer
HALAVEN (eribulin mesylate) Injection is indicated for the treatment of patients with metastatic breast cancer (mBC) who have previously received at least 2 chemotherapeutic regimens for the treatment of metastatic disease. Prior therapy should have included an anthracycline and a taxane in either the adjuvant or metastatic setting.
Liposarcoma
HALAVEN is indicated for the treatment of patients with unresectable or metastatic liposarcoma who have received a prior anthracycline-containing regimen.
Indications
Metastatic Breast Cancer
HALAVEN (eribulin mesylate) Injection is indicated for the treatment of patients with metastatic breast cancer (mBC) who have previously received at least 2 chemotherapeutic regimens for the treatment of metastatic disease. Prior therapy should have included an anthracycline and a taxane in either the adjuvant or metastatic setting.
Liposarcoma
HALAVEN is indicated for the treatment of patients with unresectable or metastatic liposarcoma who have received a prior anthracycline-containing regimen.
Important Safety Information
Warnings and Precautions
Neutropenia: Severe neutropenia (ANC <500/mm3) lasting >1 week occurred in 12% of patients with mBC and liposarcoma or leiomyosarcoma. Febrile neutropenia occurred in 5% of patients with mBC and 2 patients (0.4%) died from complications. Febrile neutropenia occurred in 0.9% of patients with liposarcoma or leiomyosarcoma, and fatal neutropenic sepsis occurred in 0.9% of patients. Patients with mBC with elevated liver enzymes >3 × ULN and bilirubin >1.5 × ULN experienced a higher incidence of Grade 4 neutropenia and febrile neutropenia than patients with normal levels. Monitor complete blood cell counts prior to each dose, and increase the frequency of monitoring in patients who develop Grade 3 or 4 cytopenias. Delay administration and reduce subsequent doses in patients who experience febrile neutropenia or Grade 4 neutropenia lasting >7 days.
Peripheral Neuropathy: Grade 3 peripheral neuropathy occurred in 8% of patients with mBC (Grade 4=0.4%) and 22% developed a new or worsening neuropathy that had not recovered within a median follow-up duration of 269 days (range 25-662 days). Neuropathy lasting >1 year occurred in 5% of patients with mBC. Grade 3 peripheral neuropathy occurred in 3.1% of patients with liposarcoma and leiomyosarcoma receiving HALAVEN and neuropathy lasting more than 60 days occurred in 58% (38/65) of patients who had neuropathy at the last treatment visit. Patients should be monitored for signs of peripheral motor and sensory neuropathy. Withhold HALAVEN in patients who experience Grade 3 or 4 peripheral neuropathy until resolution to Grade 2 or less.
Embryo-Fetal Toxicity: HALAVEN can cause fetal harm when administered to a pregnant woman. Advise females of reproductive potential to use effective contraception during treatment with HALAVEN and for at least 2 weeks following the final dose. Advise males with female partners of reproductive potential to use effective contraception during treatment with HALAVEN and for 3.5 months following the final dose.
QT Prolongation: Monitor for prolonged QT intervals in patients with congestive heart failure, bradyarrhythmias, drugs known to prolong the QT interval, and electrolyte abnormalities. Correct hypokalemia or hypomagnesemia prior to initiating HALAVEN and monitor these electrolytes periodically during therapy. Avoid in patients with congenital long QT syndrome.
Adverse Reactions
In patients with mBC receiving HALAVEN, the most common adverse reactions (≥25%) were neutropenia (82%), anemia (58%), asthenia/fatigue (54%), alopecia (45%), peripheral neuropathy (35%), nausea (35%), and constipation (25%). Febrile neutropenia (4%) and neutropenia (2%) were the most common serious adverse reactions. The most common adverse reaction resulting in discontinuation was peripheral neuropathy (5%).
In patients with liposarcoma and leiomyosarcoma receiving HALAVEN, the most common adverse reactions (≥25%) reported in patients receiving HALAVEN were fatigue (62%), nausea (41%), alopecia (35%), constipation (32%), peripheral neuropathy (29%), abdominal pain (29%), and pyrexia (28%). The most common (≥5%) Grade 3-4 laboratory abnormalities reported in patients receiving HALAVEN were neutropenia (32%), hypokalemia (5.4%), and hypocalcemia (5%). Neutropenia (4.9%) and pyrexia (4.5%) were the most common serious adverse reactions. The most common adverse reactions resulting in discontinuation were fatigue and thrombocytopenia (0.9% each).
Use in Specific Populations
Lactation: Because of the potential for serious adverse reactions in breastfed infants from eribulin mesylate, advise women not to breastfeed during treatment with HALAVEN and for 2 weeks after the final dose.
Hepatic and Renal Impairment: A reduction in starting dose is recommended for patients with mild or moderate hepatic impairment and/or moderate or severe renal impairment.
References: 1. HALAVEN [package insert]. Nutley, NJ: Eisai Inc. 2. Towle MJ, Salvato KA, Budrow J, et al. Eribulin induces irreversible mitotic blockade: implications of cell-based pharmacodynamics for in vivo efficacy under intermittent dosing conditions. Cancer Res. 2011;71(2):496-505. 3. Kuznetsov G, Towle MJ, Cheng H, et al. Induction of morphological and biochemical apoptosis following prolonged mitotic blockage by halichondrin B macrocyclic ketone analog E7389. Cancer Res. 2004;64(16):5760-5766. 4. Jordan MA, Kamath K, Manna T, et al. The primary antimitotic mechanism of action of the synthetic halichodrin E7389 is suppression of microtubule growth. Mol Cancer Ther. 2005;4(7):1086-1095. 5. Funahashi Y, Okamoto K, Adachi Y, et al. Eribulin mesylate reduces tumor microenviroment abnormality by vascular remodeling in preclinical human breast cancer models. Cancer Sci. 2014;105(10):1334-1342. 6. Dybdal-Hargreaves NF, Risinger AL, Mooberry SL. Eribulin mesylate: mechanism of action of a unique microtubule-targeting agent. Clin Cancer Res. 2015;21(11):2445-2452. 7. Jiang J, Tang YL, Liang XH. EMT: a new vision of hypoxia promoting cancer progression. Cancer Biol Ther. 2011;11(8):714-723. 8. Yoshida T, Ozawa Y, Kimura T, et al. Eribulin mesilate suppresses experimental metastasis of breast cancer cells by reversing phenotype from epithelial–mesenchymal transition (EMT) to mesenchymal–epithelial transition (MET) states. Br J Cancer. 2014;110(6):1497-1505.